Introduction
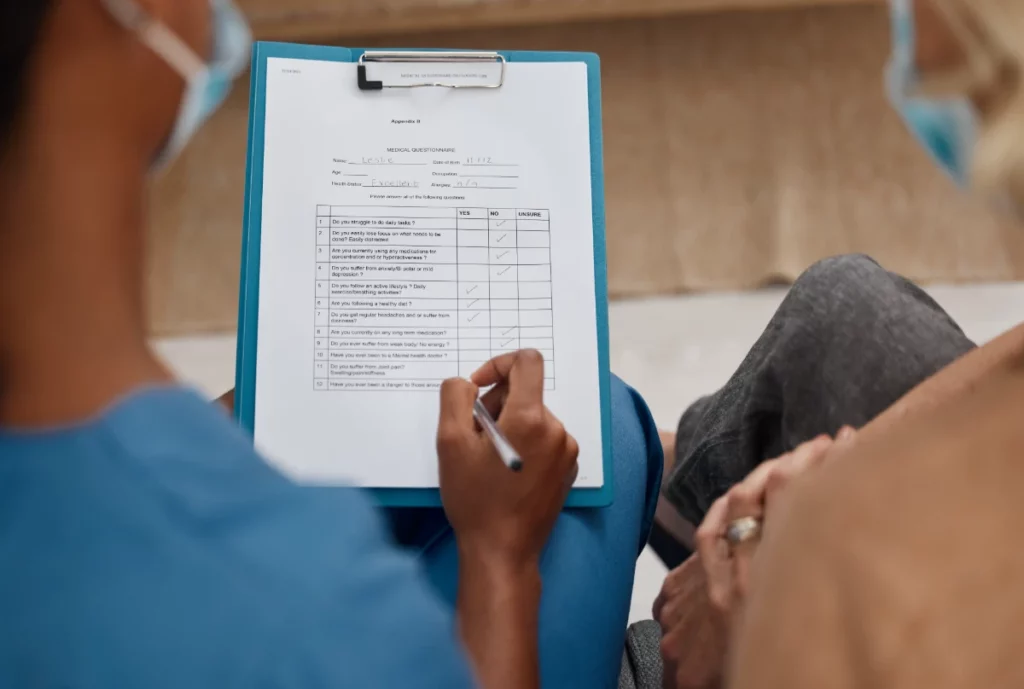
In healthcare, patient care often focuses on immediate, life-saving interventions. However, an often overlooked aspect of quality care is accurate clinical documentation. When providers are immersed in diagnosing and treating pressing health issues, documentation of seemingly minor conditions or comorbidities may seem like an afterthought. But in reality, thorough and precise documentation has a profound impact on patient outcomes, hospital performance, and financial reimbursement.
In this article, we’ll explore why clinical documentation improvement (CDI) activities should not be seen as a secondary task but as an essential part of healthcare that benefits both patients and providers.
#1 Accurate Clinical Documentation Often Takes a Backseat
It’s easy to see why accurate documentation can be overlooked. When a patient is in distress, both they and their clinician are hyper-focused on resolving the chief complaint. A patient with heart failure, for instance, may not care whether their concurrent diabetes or renal disease is meticulously documented. Similarly, a clinician may prioritize symptom relief and stabilization over painstakingly recording these comorbidities.
Yet, failing to capture these details could lead to misunderstood patient complexity, incorrect coding for reimbursement, and future gaps in care. The human aspect of care—vital as it is—can sometimes overshadow the importance of documentation, but these two aspects of patient care are deeply interconnected.
#2 The Hidden Impact of Poor Clinical Documentation
While the most immediate concern is patient relief, poor clinical documentation can lead to far-reaching consequences.
- Missed Comorbidities: Conditions not recorded during initial patient visits may remain invisible to other clinicians treating the same patient in the future.
- Inaccurate Coding: Billing depends on precise coding of patient diagnoses. Without capturing the complexity of a patient’s health, the hospital may receive lower reimbursement.
- Impaired Long-Term Care: Missing documentation today could result in misguided care tomorrow if the patient’s full health picture isn’t visible.
In the long run, these gaps in documentation impact hospital rankings, quality scores, and, most importantly, patient safety.
#3 Accurate Documentation and Risk Adjustment
A critical yet underappreciated benefit of accurate documentation is its influence on risk adjustment, which is used to predict a patient’s expected outcomes, including mortality. Proper documentation allows hospitals to reflect the complexity of their patient population more accurately.
1. Risk-Adjusted Mortality Metrics
Mortality metrics often compare observed mortality (actual deaths) to expected mortality (predicted deaths based on patient risk factors). These risk factors include age, comorbidities, and the severity of illness. By thoroughly documenting all relevant conditions, hospitals ensure a more accurate picture of their patients’ health.
For example, if a patient with severe chronic illnesses is admitted for pneumonia but their comorbidities are not fully documented, the hospital’s expected mortality for this case will be too low. If the patient then dies, the mortality metric would show an unfavorable gap between expected and observed mortality, painting an inaccurate picture of the hospital’s quality of care.
2. The Observed vs. Expected Mortality
When CDI efforts improve, expected mortality aligns better with the severity of illness. This allows for more accurate comparisons between expected and observed mortality. A hospital that consistently documents patients’ complexities will show better mortality outcomes even if the number of deaths remains unchanged. Essentially, better documentation translates to better metrics.
3. Impact on Hospital Rankings
Several widely known ranking systems—like U.S. News & World Report and CMS Hospital Compare—use risk-adjusted mortality as a key metric. Hospitals that capture the true complexity of their patients’ conditions through accurate documentation tend to score better in these rankings, leading to improved public perception and the ability to attract more patients.
“CDI efforts have the potential to elevate hospital rankings by capturing a more accurate picture of patient care,” notes a report from CMS on Hospital Value-Based Purchasing.
#4 Accurate Clinical Documentation Improves Patient Care
Beyond metrics, accurate documentation plays a crucial role in improving patient outcomes. It supports better care by ensuring that future providers have a comprehensive medical history to refer to, which is critical when making treatment decisions.
1. Future Care and Predictive Models
Data from clinical documentation is fed into predictive models used to forecast patient outcomes, such as readmission rates, expected mortality, and length of stay. By thoroughly documenting every aspect of a patient’s condition, hospitals create more reliable data for these models, translating to better care.
2. Ethical Considerations in CDI
One risk of focusing CDI efforts only on patients who pass away is that it can lead to unethical practices or a perception of “gaming” the system. If a hospital’s CDI efforts are aimed solely at improving mortality metrics, it may look like they’re trying to improve rankings rather than genuinely improving care.
On the other hand, a hospital that focuses on all patients, not just those with poor outcomes, shows a commitment to comprehensive care. Ethical CDI practices benefit patients by improving outcomes, documentation, and hospital performance metrics.
#5 Financial and Regulatory Benefits of Accurate Clinical Documentation
The implications of thorough documentation stretch far beyond patient care and into the realms of financial reimbursement and regulatory compliance.
1. Compliance and Reimbursement
Accurate documentation is essential for appropriate billing and reimbursement. When a patient’s condition is properly documented, it ensures that hospitals are compensated based on the actual complexity of care provided. This is particularly critical in today’s healthcare environment, where reimbursement is often tied to quality metrics like mortality rates.
For instance, the CMS Value-Based Purchasing Program adjusts hospital payments based on their performance in areas like mortality and readmissions. Inadequate documentation can lead to reimbursement penalties under programs like the Readmissions Reduction Program or the Hospital-Acquired Conditions Reduction Program, even if the care provided was appropriate.
2. Preventing Complications and Readmissions
Documentation also impacts how hospitals manage complications and readmissions. Properly recorded patient information can help prevent future hospitalizations by ensuring that all comorbidities are treated—even those that don’t seem immediately pressing. This, in turn, improves patient outcomes and reduces the hospital’s risk of financial penalties.
Conclusion
Accurate clinical documentation may seem like a background task in pressing medical emergencies, but it is critical in determining patient outcomes, hospital performance, and financial reimbursement. Comprehensive documentation supports better patient care, ensures ethical CDI practices, and directly impacts metrics like expected mortality and hospital rankings.
Hospitals create a culture of continuous improvement and accountability by prioritizing documentation improvement for all patients, not just those with poor outcomes. Ultimately, this leads to safer patient care and better results across the healthcare system.
Improving clinical documentation requires a systematic approach, and quality improvement (QI) tools are essential for driving change in this area. These tools help healthcare teams identify inefficiencies, streamline processes, and ensure that documentation captures the full complexity of patient care. By using established QI frameworks, hospitals can build a culture of continuous improvement around documentation, ensuring it remains a priority alongside direct patient care.
Key Takeaways:
- Accurate documentation improves risk adjustment, leading to better mortality metrics.
- It affects financial incentives under programs like CMS Value-Based Purchasing.
- Comprehensive CDI efforts benefit patient outcomes, hospital rankings, and public perception.
The bottom line: Clinical documentation is not just a paperwork exercise—it’s a powerful tool that, when done right, enhances the quality of care for every patient.
For more in-depth discussions on patient safety and clinical best practices, check out our resources at www.patientsafetyexperts.com.