Introduction:
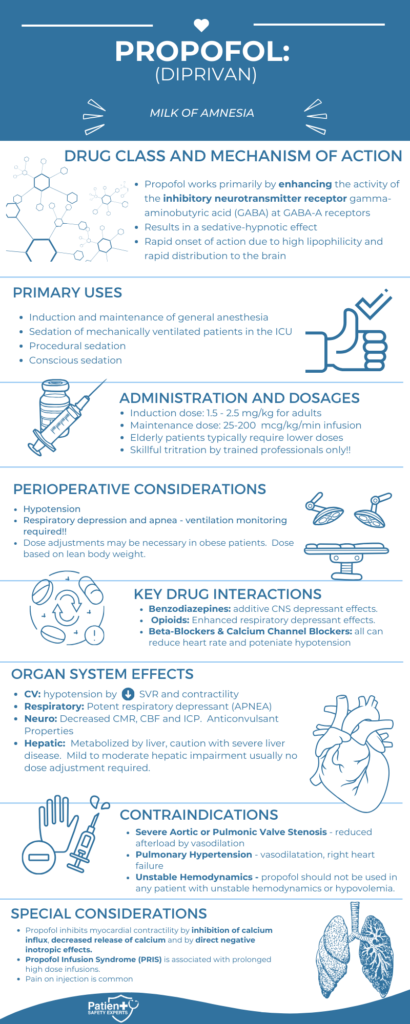
Propofol, known by its generic name and brand names like Diprivan and Propoven, is a widely used intravenous anesthetic agent. It plays a crucial role in various medical procedures, offering both induction and maintenance of anesthesia with a rapid onset and short duration of action. Due to its unique pharmacologic properties, Propofol is often the anesthetic of choice in many clinical settings.
Pharmacologic Overview:
Propofol is a short-acting anesthetic that works primarily by enhancing the activity of gamma-aminobutyric acid (GABA) at GABA_A receptors in the brain. This action results in sedation, hypnosis, and decreased pain perception. The drug’s high lipid solubility allows it to quickly cross the blood-brain barrier, leading to a rapid onset of action, typically within 30-40 seconds. Propofol is metabolized in the liver and excreted through the kidneys, with a short context-sensitive half-life, making it suitable for continuous infusions.
Common and Uncommon Uses:
Propofol is predominantly used for the induction and maintenance of general anesthesia. Its rapid onset and smooth recovery profile make it ideal for both inpatient and outpatient procedures. Additionally, Propofol is widely utilized for sedation in the intensive care unit (ICU), procedural sedation during endoscopy or colonoscopy, and even conscious sedation for minor medical procedures.
Beyond these common uses, Propofol has found a place in less typical scenarios, such as treating refractory status epilepticus and providing sedation for radiation therapy or diagnostic imaging.
Dosage and Administration:
The administration of Propofol varies depending on the intended use:
- Induction of Anesthesia: Adults typically receive 1.5-2.5 mg/kg, while children may require 2.5-3.5 mg/kg.
- Sedation: An initial dose of 0.5-1 mg/kg, followed by a continuous infusion of 25-75 mcg/kg/min, is common.
Given its potent effects, careful titration is essential, especially in vulnerable populations like the elderly, who require lower doses due to increased sensitivity and decreased clearance.
Organ System Effects and Perioperative Implications:
Propofol’s effects span multiple organ systems, each with its own set of considerations:
- Central Nervous System: Propofol induces rapid loss of consciousness and sedation but can cause significant CNS depression. Monitoring for postoperative delirium, particularly in elderly patients, is critical.
- Cardiovascular System: Propofol can cause hypotension by reducing systemic vascular resistance (SVR) and cardiac output. Close blood pressure monitoring, especially in patients with compromised hemodynamics, is essential, and vasopressors may be needed.
- Respiratory System: As a potent respiratory depressant, Propofol can cause apnea during induction, necessitating airway management and oxygen supplementation.
- Hepatic and Renal Systems: While Propofol is metabolized in the liver, hepatic dysfunction generally does not significantly affect its clearance. In renal impairment, however, caution is advised to avoid drug accumulation.
- Musculoskeletal System: Myoclonus and involuntary movements can occur during induction, usually transient and self-limiting.
- Immune System: A rare but severe complication is propofol-related infusion syndrome (PRIS), particularly with prolonged high-dose infusions, characterized by metabolic acidosis, rhabdomyolysis, and cardiac failure.
Drug-Drug Interactions:
Propofol’s effects can be potentiated by other medications commonly used during surgery, such as benzodiazepines, opioids, and inhalational anesthetics, increasing the risk of respiratory depression and hypotension. Due to additive effects, caution is also required when combining Propofol with neuromuscular blocking agents, beta-blockers, and calcium channel blockers.
Perioperative Risks and Implications:
Propofol’s primary perioperative risks include hypotension, respiratory depression, and the potential for bacterial contamination due to its lipid-based emulsion. Prolonged infusions carry the risk of PRIS, necessitating vigilant monitoring for signs of metabolic acidosis, rhabdomyolysis, and heart failure.
Special Considerations:
Propofol requires dose adjustments based on the patient’s age and weight. For instance, children typically need higher doses per kilogram, while the elderly require lower doses due to increased sensitivity. In obese patients, dosing should be based on lean body weight to avoid overdose.
Contraindications and FDA Warnings:
Absolute contraindications for Propofol include known hypersensitivity to the drug or its components and a history of PRIS. Relative contraindications include severe cardiac disease, hypotension, and disorders of fat metabolism. Although there are no black box warnings for Propofol, recent advisories emphasize the importance of aseptic handling and monitoring for PRIS during prolonged infusions.
Conclusion:
Propofol remains a cornerstone in modern anesthesia practice due to its rapid onset, short duration, and versatile application across various medical procedures. However, its use requires careful monitoring and understanding of its potential interactions and complications to ensure patient safety and optimal outcomes.
Other Intravenous Induction Agents:
- Etomidate
- Ketamine
- Methohexital
- Thiopental
- Midazolam